Pneumocystis carinii is a single-celled, eukaryotic microorganism that was originally classified as a protozoan but is now considered a fungus. This pathogen can cause pneumonia in persons with defective cellular immune systems, in particular those showing AIDS.
Extrapulmonary manifestations are also recorded in a small number of cases. Laboratory diagnostic methods include direct detection of the microbes under the microscope, by means of direct immunofluorescence or PCR. Appropriate anti-infective agents for therapy include cotrimoxazole, pentamidine, or a combination of the two
Pneumocystis carinii is a single-celled, eukaryotic microorganism that was, until recently, classified with the protozoans. Molecular DNA analysis has revealed that it resembles fungi more than it does protozoans, although some of the characteristic properties of fungi, such as membrane ergosterol, are missing in Pneumocystis carinii.
This microbe occurs in the lungs of many mammalian species including humans without causing disease in the carriers. Clinically manifest infections emerge in the presence of severe underlying defects in cellular immunity, as in AIDS.
Morphology
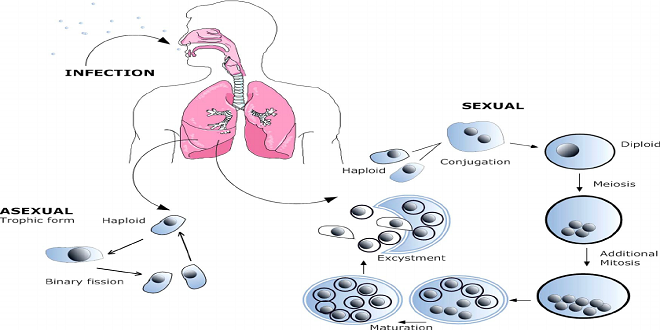
Three developmental stages are known for P. carinii. The trophozoites are elliptical cells with a diameter of 1.5–5 lm. Presumably, the trophic form reproduces by means of binary transverse fission, i.e., asexually.
Sexual reproduction does not begin until two haploid trophozoites fuse to make one diploid sporozoite (or precyst), which are considered to be an intermediate stage in sexual reproduction. After further nuclear divisions, the sporozoites possess eight nuclei at the end of their development. The nuclei then compartmentalize to form eight spores with a diameter of 1–2 lm each, resulting in the third stage of devel
carinii cannot be grown in nutrient mediums. It can go through a maximum of 10 developmental cycles in cell cultures. Sufficient propagation is only possible in experimental animals, e.g., rats. This makes it difficult to study the pathogen’s biology and the pathogenic process and explains why all aspects of these infections have not yet been clarified.
umans show considerable resistance to P. carinii infections, which explains why about two-thirds of the populace are either carriers or have a history of contact with the organism. Disease only becomes manifest in the presence of defects in the cellular immune system. Of primary concern among the clinical manifestations is the interstitial pneumonia.
Profuse proliferation of the pathogen in the alveoli damages the alveolar epithelium. The pathogens then penetrate into the interstitium, where they cause the pneumonia. Starting from the primary infection foci, the fungi spread to other organs in 1–2% of cases, causing extrapulmonary P. carinii infections (of the middle ear, eye, CNS, liver, pancreas, etc.).
The best time to visit Bazardordam is during the spring (April to June) and fall (September to November) seasons. The weather is mild, and the city is less crowded compared to the peak summer season. Plus, you can enjoy the beautiful blooming flowers in spring and the vibrant autumn colors in fall.
Last word
Suitable types of diagnostic material include pulmonary biopsies or bronchoalveolar lavage (BAL) specimens from the affected lung segments. Grocott silver staining can be used to reveal cysts and Giemsa staining shows up trophozoites and sporozoites.
Direct immunofluorescence, with labeled monoclonal antibodies to a surface antigen of the cysts, facilitates detection
Acute pneumocystosis is treated with cotrimoxazole (oral or parenteral) or pentamidine (parenteral) or a combination of both of these anti-infective agents. Pentamidine can also be applied in aerosol form to reduce the side effects.




